Think of your immune system as a painstaking internal task force that is constantly on the lookout for bacterial invasions, viral threats, and cellular anomalies. Imagine that force, which is so well-trained and typically reliable, suddenly attacking its own headquarters. For people with autoimmune diseases, that is the reality: a startlingly contradictory situation in which the body’s defense systems mistakenly perceive healthy tissue as hostile invaders.
In the United States alone, an estimated 24 million people suffer from these remarkably varied and increasingly prevalent conditions. There are over 100 types known to exist, and symptoms can vary from mild fatigue to systemic failure affecting the entire body. Despite the complexity, there is hope because many patients’ quality of life has significantly improved thanks to contemporary treatments that are fueled by precision medicine and immunological research.
Key Insights About Autoimmune Disease
| Aspect | Details |
|---|---|
| Definition | An illness where the immune system mistakenly attacks the body’s healthy cells and tissues |
| Common Symptoms | Fatigue, joint pain, inflammation, digestive issues, skin rashes, neurological changes |
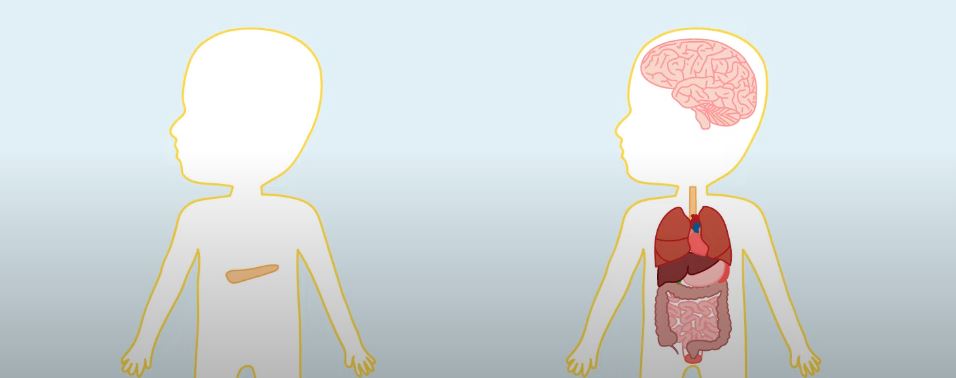
| Frequent Targets | Skin, joints, glands, nerves, intestines, thyroid, pancreas |
| Representative Conditions | Lupus, Multiple Sclerosis (MS), Rheumatoid Arthritis (RA), Psoriasis, Crohn’s, Type 1 Diabetes |
| Prevalence | 1 in 15 people; 78% of cases affect women |
| Noted Triggers | Infections, genetic predisposition, pollutants, stress, diet, medications |
| Standard Treatments | Steroids, biologics, immunosuppressants, anti-inflammatories, lifestyle adjustments |
| Credible Source | Cleveland Clinic – Autoimmune Disease |
When the Body Misfires: An Extremely Disadvantageous Friendly Fire Situation
A remarkably misunderstood biological error is the root cause of autoimmune diseases. The immune system, which is typically trained to recognize and eliminate infections, becomes perplexed. It releases immune cells and antibodies that start attacking your internal organs, joints, or skin because they believe they are dangers. This behavior stems from malfunctioning cellular memory and is not random.
Doctors are now able to identify autoimmune patterns earlier thanks to diagnostic insights gathered over decades of research, which provides patients with the means to control flare-ups, maintain function, and prevent additional tissue damage.
What Causes the Immune System to Act Out of Control?
Although there isn’t a single, all-encompassing solution, a number of overlapping theories have been proposed. When environmental triggers like chemical exposure or viral infections are coupled with genetic predisposition, the immune system may be primed to respond improperly. When hormonal changes and ongoing stress are involved, flare-ups frequently happen suddenly.
Some populations are more susceptible to certain autoimmune diseases, such as lupus or Hashimoto’s thyroiditis. A disproportionate number of women are impacted, especially those who are fertile. Certain illnesses, like rheumatoid arthritis, seem to run in families, indicating a definite genetic component.
Managing an Autoimmune Disease: Transitioning from Illness to Function
Symptoms of autoimmune disease frequently appear in waves, sometimes mild and other times severe. Morning joint stiffness, persistent exhaustion, or unexpected stomach problems may not seem connected, but systemic inflammation frequently connects them. Doctors call these cycles of remission and relapse “flares.”
Many people attain long-term stability by managing their health and making thoughtful lifestyle changes. Targeted biologic medications, physical therapy, nutrient-focused diets, and stress-reduction strategies are frequently included in customized regimens—tools that turn surviving into thriving.
The Way Forward: A Future Characterized by Accuracy and Hope
Deeper immunological mechanisms will likely be revealed by medical research in the upcoming years, possibly enabling the early detection of disease symptoms. Two particularly cutting-edge methods being studied in clinical settings are AI-assisted diagnostics and microbiome manipulation. Trials for lupus and multiple sclerosis are already showing encouraging results from precision medicine, which customizes treatment based on a patient’s genetic and immunological profile.
Healthcare providers can now offer treatment options that were previously unthinkable by combining genomic data with real-time symptom tracking.
FAQs – Autoimmune Disease in Brief
What is an autoimmune disease?
A disorder where the immune system attacks healthy cells by mistake.
What are the common signs?
Fatigue, joint pain, inflammation, skin changes, gut issues.
Is it curable?
No cure yet, but symptoms can be managed effectively.
Who’s at risk?
Women, people with family history, or past infections.
How is it diagnosed?
Via blood tests, imaging, and autoimmune markers.
Can it go away on its own?
Usually chronic, but symptoms may go into remission.
Does diet matter?
Yes—anti-inflammatory foods may reduce flare severity.
Is stress a factor?
Definitely. Stress can trigger or worsen flares.
How many types exist?
Over 100, ranging from mild to life-threatening.
Is treatment lifelong?
Most patients require ongoing care, but outcomes are improving.

1 Comment
Pingback: Gastroesophageal Reflux Disease and Your Sleep - The Shocking Link That’s Ruining Your Rest - Route to Resilience Health UK